Living with Stiff-person Syndrome: A Personal Journey of Strength and Resilience
Imagine waking up one day only to find that your body has become stiff, rigid, and seemingly unyielding. Simple tasks like walking or reaching for a cup of coffee suddenly feel like insurmountable challenges. This is the reality for individuals living with Stiff-person Syndrome (SPS), a rare neurological disorder that tests both physical strength and emotional resilience.
In this blog post, we will delve into the intricacies of Stiff-person Syndrome – what it is, how it affects those who have it, and the remarkable stories of individuals who navigate life’s twists and turns with unwavering determination. Join us on this journey as we shed light on this often misunderstood condition while celebrating the indomitable spirit that propels these warriors forward against all odds. So grab a cuppa, settle in comfortably, and let’s embark on an inspiring exploration into the world of Stiff-person Syndrome!
What is Stiff-person Syndrome?
Stiff-person Syndrome (SPS) is a rare neurological disorder that affects the muscles and causes extreme stiffness and spasms. It is characterized by episodes of muscle rigidity, which can make movement difficult or even impossible. SPS primarily targets the trunk muscles, making it challenging to walk, sit, or perform everyday activities.
This condition arises from an autoimmune response where the body’s immune system mistakenly attacks the neurons responsible for muscle control. As a result, individuals with Stiff-person Syndrome often experience debilitating pain and involuntary muscle contractions that can be triggered by stress, sudden movements, or emotional distress. Living with this syndrome requires immense strength and resilience in navigating through life’s obstacles while finding ways to manage its symptoms effectively.
Disease Overview
Stiff-person Syndrome, also known as SPS, is a rare and chronic neurological disorder that affects the muscles and movement of the body. It falls under the category of autoimmune diseases, where the immune system mistakenly attacks healthy cells.
This condition primarily affects the central nervous system, leading to muscle stiffness and spasms that can be debilitating for those living with it. The severity of symptoms can vary from person to person, making each individual’s experience unique. Stiff-person Syndrome is a complex disease that requires careful management and understanding to navigate its challenges effectively
Signs and Symptoms
Stiff-person Syndrome can be a challenging condition to live with, as it presents a range of signs and symptoms that can vary in severity from person to person. One of the hallmark features of this syndrome is muscle stiffness, which typically affects the trunk muscles but can also involve other parts of the body. This stiffness often leads to difficulty with movement and mobility.
In addition to muscle stiffness, individuals with Stiff-person Syndrome may experience muscle spasms or involuntary contractions. These spasms can be painful and disruptive, further impacting daily activities. Other common symptoms include heightened sensitivity to touch or noise, anxiety or panic attacks, and an exaggerated startle response. It’s important for individuals experiencing these symptoms to consult with a healthcare professional for proper diagnosis and management strategies.
Understanding Stiff-person Syndrome
Stiff-person Syndrome is a rare neurological disorder that can significantly impact a person’s quality of life. Understanding this condition is essential for effective management and support.
Compared to other forms of stiffness, Stiff-person Syndrome involves muscle rigidity and spasms that are often triggered by stress or sudden movements. It can cause difficulty in walking, balance issues, and even result in falls. While the exact cause is unknown, researchers believe it may involve an autoimmune response affecting the nervous system.
Individuals who are more likely to develop Stiff-person Syndrome include those with a family history of autoimmune disorders or certain genetic mutations. Women are also at a higher risk than men. Early diagnosis and prompt treatment play crucial roles in managing symptoms and improving outcomes for individuals living with this challenging condition.
How does it compare to other forms of stiffness?
Stiff-person Syndrome is a rare neurological disorder characterized by muscle stiffness and spasms. While it shares some similarities with other forms of stiffness, such as muscle cramps or rigidity caused by conditions like Parkinson’s disease, there are distinct differences that set Stiff-person Syndrome apart.
One key difference is the intensity and persistence of the stiffness in Stiff-person Syndrome. Unlike temporary muscle cramps or occasional rigidity seen in other conditions, individuals with Stiff-person Syndrome experience continuous and severe muscle stiffness that can significantly impair their mobility and quality of life. This constant state of tension sets it apart from more transient forms of stiffness.
Furthermore, the triggers for symptoms differ between Stiff-person Syndrome and other types of stiffness. In common cases like exercise-induced cramps or stress-related tension, the symptoms arise due to specific external factors. However, in Stiff-person Syndrome, these triggers may not be apparent or easily identifiable. The onset of symptoms can occur randomly without any obvious cause, further distinguishing this condition from others.
With its unique characteristics and unpredictable nature, living with Stiff-person Syndrome presents its own set of challenges for those affected. Understanding these distinctions helps healthcare professionals tailor treatment plans specifically to address the complex needs associated with this rare condition.
Who is more likely to get Stiff-person Syndrome?
Stiff-person Syndrome is a rare neurological disorder that can affect anyone, regardless of age or gender. While the exact cause of this condition remains unknown, certain risk factors have been identified. It is believed that individuals with a family history of autoimmune diseases may be at a higher risk for developing Stiff-person Syndrome. Additionally, certain genetic predispositions and hormonal imbalances may also play a role.
Furthermore, it has been observed that Stiff-person Syndrome tends to occur more frequently in women than men. However, this could be due to underdiagnosis in men rather than an actual difference in prevalence between genders. More research is needed to fully understand the specific factors that contribute to the development. Stiff-person Syndrome and why certain individuals are more likely to be affected by this challenging condition
Diagnosis and Treatment
How is Stiff-person Syndrome diagnosed? It can be challenging to diagnose Stiff-person Syndrome due to its rarity and similarity to other neurological conditions. Diagnosis typically involves a thorough medical history, physical examination, and various tests. These may include blood tests, electromyography (EMG), nerve conduction studies, and imaging scans.
Once diagnosed with Stiff-person Syndrome, what are the treatment options? While there is no cure for this condition, treatment focuses on managing symptoms and improving quality of life. Medications such as muscle relaxants or anti-spasmodic drugs. May be prescribed to alleviate stiffness and spasms. Physical therapy can also help improve mobility and flexibility. In some cases, intravenous immunoglobulin (IVIG) therapy. Or plasma exchange may be used to suppress immune system activity. A multidisciplinary approach involving healthcare professionals specializing in neurology, rheumatology, physiotherapy. Occupational therapy, psychology, and pain management is often recommended for comprehensive care.
How is Stiff-person Syndrome diagnosed?
Diagnosing Stiff-person Syndrome (SPS) can be a complex process. As its symptoms are often mistaken for other conditions. To determine if someone has SPS, doctors typically rely on a combination of clinical evaluation and specialized tests. During the examination, medical professionals will assess muscle stiffness, spasms, and rigidity in different parts of the body. They may also ask detailed questions about symptoms and medical history to rule out other possible causes.
To confirm a diagnosis, specific laboratory tests may be ordered. These can include blood tests to check for elevated levels of certain antibodies associated with SPS or neurochemicals that play a role in nerve signaling. Electromyography (EMG), which measures electrical activity in muscles, can provide further insights into muscle dysfunction and hyperexcitability commonly seen in SPS patients. Accurate diagnosis is crucial for developing an appropriate treatment plan and managing the condition effectively.
What are the treatment options?
When it comes to treating Stiff-person Syndrome, a tailored approach is essential. While there is no cure for this rare neurological disorder, various treatment options can help manage the symptoms and improve quality of life.
One common treatment option is medication. Doctors may prescribe muscle relaxants or anti-anxiety medications to alleviate stiffness and muscle spasms. In some cases, immunosuppressive drugs like diazepam or baclofen are also used to reduce nerve activity.
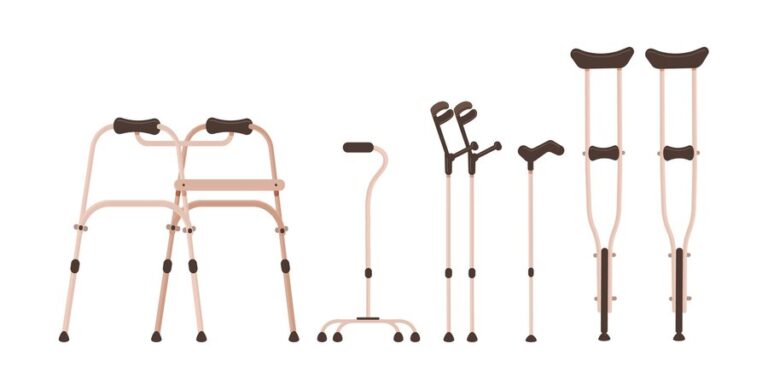
Physical therapy can play a crucial role in managing Stiff-person Syndrome as well. Therapists can design exercise programs that focus on stretching and strengthening muscles, improving flexibility and mobility. Assistive devices such as braces or walkers may be recommended to aid in walking and balance.
Remember, every individual with Stiff-person Syndrome will have different needs. So treatment plans must be personalized accordingly. It’s important to consult with healthcare professionals who specialize in this condition to determine the most suitable options for each person’s unique circumstances!
Living with Stiff-person Syndrome
Living with Stiff-person Syndrome can be a constant battle, both physically and emotionally. Every day brings its own set of challenges, as the body becomes stiff and rigid, making even simple tasks seem insurmountable. The limitations imposed by this rare neurological disorder can be frustrating and isolating.
However, despite the difficulties faced by individuals living with Stiff-person Syndrome, there is an incredible strength and resilience that shines through. It is awe-inspiring to witness their determination to adapt and find ways to live fulfilling lives despite the obstacles they face on a daily basis. With unwavering courage, they navigate through life’s ups and downs, refusing to let their condition define them.
In their journey of living with Stiff-person Syndrome, these remarkable individuals not only exemplify perseverance but also inspire others around them. Their stories serve as a reminder that no matter how challenging life may become, there is always room for hope and possibility. They teach us the importance of embracing our inner strength in times of adversity and cherishing every small victory along the way. Living with Stiff-person Syndrome requires immense courage – it is a testament to human resilience in its purest form.
Managing Symptoms
Living with Stiff-person Syndrome can be challenging, but there are ways to manage the symptoms and improve quality of life. One important aspect is medication. Doctors may prescribe medications such as diazepam or baclofen to help relax muscles and reduce stiffness. These medications can provide temporary relief and make daily activities more manageable.
In addition to medication, physical therapy can also play a crucial role in symptom management. Working with a physical therapist who understands the unique challenges of Stiff-person Syndrome can help individuals develop exercises and stretches that target specific muscle groups affected by the condition. Regular stretching routines can promote flexibility and mobility, easing stiffness and improving overall function.
Remember, managing symptoms is an ongoing process that may require adjustments over time. It’s important for individuals living with Stiff-person Syndrome to work closely with their healthcare team to find the most effective treatment plan for their specific needs. By staying proactive in symptom management, it’s possible to maximize functionality and maintain a higher quality of life despite the challenges posed by this rare neurological disorder.
Lifestyle Modifications
Living with Stiff-person Syndrome can present numerous challenges, but there are lifestyle modifications that individuals can implement to help manage their symptoms and improve their overall quality of life. Adapting to a new way of living may require some adjustments, but with determination and resilience, it is possible to find strategies that work for each individual.
One important aspect of lifestyle modification is creating an environment that supports physical independence and safety. This may involve making modifications within the home such as installing handrails or ramps, using assistive devices like walkers or wheelchairs when needed, and ensuring accessibility throughout the living space. Additionally, practicing good ergonomics in daily activities such as sitting or standing posture can help alleviate muscle stiffness and discomfort.
Maintaining a healthy lifestyle through regular exercise is also crucial for managing Stiff-person Syndrome. Engaging in low-impact exercises like swimming or gentle stretching routines can help improve flexibility and reduce muscle rigidity. It’s essential to consult with healthcare professionals specializing in this condition before starting any exercise program to ensure safety.
Remember that everyone’s experience with Stiff-person Syndrome will be unique, so finding what works best for you may take time. Stay positive, seek out support from loved ones and patient communities, and never hesitate to reach out for professional guidance along your journey towards strength and resilience!
Patient Support and Resources
Living with Stiff-person Syndrome can be challenging, but thankfully there are resources and support available to help patients navigate their journey. Connecting with others who understand the daily struggles can provide a much-needed sense of community and empathy. Online support groups and forums allow individuals to share experiences, ask questions, and find comfort in knowing they are not alone.
In addition to emotional support, there are also practical resources that can assist patients in managing their condition. Educational websites and publications offer valuable information on Stiff-person Syndrome, including updates on research advancements and treatment options. Physical therapy programs specifically designed for this syndrome may help improve mobility and quality of life. Accessing these patient support networks allows individuals living with Stiff-person Syndrome to gain knowledge, strength, and encouragement from others facing similar challenges every day.
Prognosis and Outlook
What is the prognosis for Stiff-person Syndrome? While it can vary from person to person, this rare neurological disorder generally has a chronic and progressive course. The severity of symptoms can fluctuate, with periods of stability followed by sudden exacerbations.
Living with Stiff-person Syndrome requires resilience and determination as individuals navigate through challenges on a daily basis. Despite the uncertainties surrounding this condition, many people find strength in their support systems and strive to maintain a positive outlook. With ongoing medical care, symptom management strategies, and emotional support, individuals living with Stiff-person Syndrome can continue to lead fulfilling lives despite the obstacles they face.
What is the prognosis for Stiff-person Syndrome?
Living with Stiff-person Syndrome can be a challenging journey, but understanding the prognosis of this rare neurological disorder is crucial for patients and their loved ones. The prognosis for Stiff-person Syndrome varies from person to person, as each case is unique. Some individuals may experience mild symptoms. That can be managed with treatment, while others may face more severe challenges in their daily lives.
Despite the unpredictable nature of the disease, it’s important to remain hopeful. With proper medical care and support, many people living with Stiff-person Syndrome are able to find ways to manage their symptoms and maintain a good quality of life. It’s essential for patients to work closely with healthcare professionals who specialize in neurology and movement disorders to develop an individualized treatment plan that addresses their specific needs. Remember, there is always hope on this journey towards strength and resilience!
Personal Stories of Strength and Resilience
Living with Stiff-person Syndrome requires immense strength and resilience. The journey can be filled with challenges, but many individuals have found ways to overcome them and live fulfilling lives.
One inspiring aspect of this condition is the personal stories of those who face it head-on. These individuals share their experiences, highlighting their courage and determination in the face of adversity. From learning to adapt to daily activities to finding joy in small victories, their stories serve as a reminder that there is hope even in the most difficult circumstances.
Through online support groups and community events, people living with Stiff-person Syndrome find solace in connecting with others who understand their struggles. They provide each other with emotional support, advice, and encouragement. Sharing personal triumphs and setbacks helps foster a sense of unity among patients who often feel isolated due to the rarity of this condition.
These personal stories not only inspire others facing similar challenges but also shed light on the importance of empathy and understanding for those dealing with Stiff-person Syndrome. Each story serves as a testament to human resilience. And reminds us all that strength can be found even in the darkest moments.
Shared experiences of individuals living with Stiff-person Syndrome
Living with Stiff-person Syndrome is undoubtedly challenging, but it is also a testament to the strength and resilience of those affected by this rare neurological disorder. Despite the physical limitations and daily struggles they face, individuals with Stiff-person Syndrome find ways to adapt, overcome, and thrive.
Each person’s journey with Stiff-person Syndrome is unique, but one thing remains constant: their unwavering determination to live life to the fullest. Through therapy, medication management, lifestyle modifications, and support from loved ones and healthcare professionals, many individuals are able to regain some control over their bodies and maintain a good quality of life.
The shared experiences of these brave individuals serve as an inspiration for others facing similar challenges. They have found solace in connecting with fellow patients through online support groups or local community organizations dedicated to raising awareness about Stiff-person Syndrome. By sharing their stories openly and honestly, they offer hope and encouragement not only to those living with the condition but also to their families and friends who may be seeking guidance on how best to support them.
These personal accounts shed light on the day-to-day realities of managing symptoms such as muscle stiffness/spasms/tremors/jerks (myoclonus), balance issues/falls/instability/gait disturbances/foot drop/slurred speech/vision problems/anxiety/depression/fatigue/painful muscle cramps/sleep disturbances. They highlight coping strategies that range from physical therapies like stretching exercises or yoga practices tailored. Specifically for people with limited mobility due to muscle rigidity/stiffness/spasticity/cramps/muscle spasms. Assistive devices such as braces/walkers/canes/wheelchairs; pain management techniques including heat therapy/topical creams/medications. Psychological counseling/support groups focusing on mental well-being/emotional resilience/stress reduction techniques. Dietary changes/supplements aimed at reducing inflammation; and alternative therapies like acupuncture/massage therapy.