Treatment options for Atopic Dermatitis
Atopic dermatitis (AD), further generally known as eczema, is a habitual skin condition that requires comprehensive treatment. This involves symptom operation, flare-up prevention, and restoration of the skin. A treatment option can range based on how severe your condition is and could be a mix of lifestyle changes or medication-based incentives.
Symptoms of atopic dermatitis are different depending upon age, the intensity of the condition, as well as which element of the body is affected.
General Overview of Atopic Dermatitis Symptoms
Atopic dermatitis generally has ages of flare-ups as well as remittals (when the symptoms go down), and these can be seen indeed in as many weeks to months. Any questions regarding what is Atopic Dermatitis, this blog has all the answers.
- Intense Itching (Pruritus)
Maybe the most distinctive and disquieting symptom of atopic dermatitis is violent itching. This itching can be severe enough to disrupt diurnal conditioning and significantly impact the quality of life. In fact, itching is considered the most distressing symptom by numerous individuals suffering from AD.
- Dry, scaly skin
Dry, scaly skin that may develop cracks in severe cases is another hallmark sign of atopic dermatitis. In those with AD, the skin fails to maintain proper hydration. The outermost layer of the skin, the epidermis, typically acts as a defensive hedge, preventing water loss and guarding against dangerous substances.
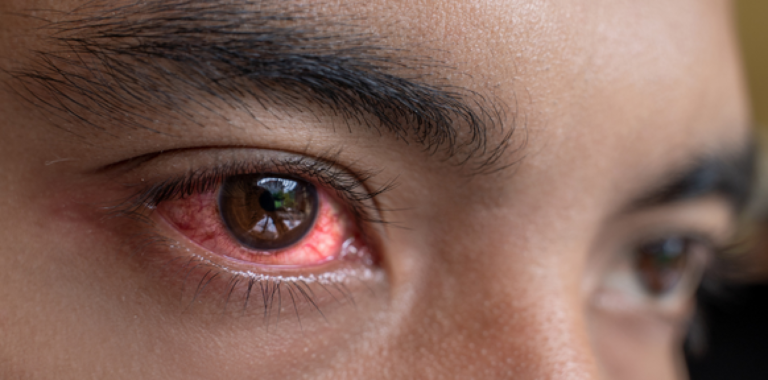
- Red or inflamed patches
The easiest thing to spot is red, inflamed patches of skin (atopic dermatitis). These patches feel hot and painful, and the edges will be distinct so that they are seen rather clearly. Normally they develop on areas of the body suitable to the age group.
- Rashes
Atopic dermatitis rashes look different in each stage. Papules or vesicles with small raised bumps (can be oozed) crust when scratched are most likely seen during acute flare-ups. These rashes are always very itchy and spread easily when treatment is neglected. UVBMEDI have light therapy for Atopic Dermatitis that can help you to get rid of this disease.
- Crusting and Oozing
In severe cases, and especially during flare-ups, the skin can get so inflamed and damaged that it weeps fluid. Crusts may start to develop at the site of scratching, and they can be yellow or brown. This oozing happens when the vesicles or blisters, which contain clear or slightly yellowish fluid, on broken skin break.
- Skin Infections
Since people with atopic dermatitis have a defective skin barrier, they’re especially vulnerable to infections of the skin. These infections are caused by bacteria, contagion, or fungus. Examples of common bacterial infections related to AD include infection by Staphylococcus aureus aggravated atopic symptoms with increased inflammation, redness, swelling, and possibly the formation of pus.
- Emotional and psychological symptoms
Chronic conditions such as atopic dermatitis also take a toll on the mental health and emotional state of the person. They could warrant confidence and develop passions of embarrassment, frustration, and indeed helplessness. Nighttime itch and sleep disturbance may lead to fatigue and perversity, as well as difficulties with memory and attention.
Treatment options for atopic dermatitis:
- Moisturizers and Skin Care
Atopic dermatitis care starts with moisturizing the skin. Regular use of emollients (moisturisers) helps to repair the skin, as blankness can beget increased symptoms. Thick, scent-free creams or ointments are stylish and can be applied straight after bathing while your skin is still moist in order to trap humidity.
- Topical Corticosteroids
Topical corticosteroids remain the standard of care for treatment of an ongoing flare. These are the anti-inflammation creams or ointments that reduce redness, lumps, and itching.
The corticosteroid strength will depend on how bad the symptoms are and where on your skin the affected area is. For thin skin areas like the face, low- to medium-potency steroids will suffice, but for thicker skinned locations (the hands or feet), a higher-potency steroid is likely necessary.
- Topical Calcineurin Inhibitors
For cases who cannot use corticosteroids or if long-term operation is necessary, topical calcineurin impediments (TCIs), including tacrolimus and pimecrolimus, can be used rather. These work to suppress the vulnerable response in the skin, dampening down inflammation and itching without lacing the skin. TCIs are typically used on sensitive areas, such as the face and around the eyes, or in people who require steroid-sparing therapy.
- Oral Medications
In cases of severe or widespread atopic dermatitis, oral medications may be necessary. These include:
- Oral corticosteroids: oral corticosteroids for acute exacerbations with avoidance of long-term remedy grounded upon side effect profile.
- Immunosuppressants: Such as cyclosporine, methotrexate, and azathioprine might be specified for severe cases of treatment-resistant psoriasis in an attempt to reduce inflammation by suppressing the vulnerable system.
- Oral antihistamines: These are not designed to treat the underpinning inflammation; still, they can give rapid-fire relief for itching (pparticularly at night) due to their sedative effect.
- Phototherapy
Phototherapy with ultraviolet (UV) light may be effective in some cases. Slows down skin cell production to reduce inflammation and itching. Light therapy for Atopic Dermatitis is used for more severe cases, mostly 3 to 7 when topical treatments are not enough.
Conclusion
Atopic dermatitis can manifest in different forms, from severe itching and short, dry skin to weeping, caked blisters, or thickened skin. The complaint frequently runs a shifting course, consisting of flare-ups and remissions. On top of all this, atopic dermatitis can affect emotional status and quality of life!